SMMC Program Changes
The Agency for Health Care Administration (“AHCA”) is responsible for administering the Statewide Medicaid Managed Care (“SMMC”) program. Most Medicaid recipients receive all their Medicaid services through the SMMC program. The following explains AHCA’s plan for communicating with Medicaid recipients to prepare them for the transition to the new SMMC plans. AHCA recently re-procured health plans for the SMMC program. These plans will provide medical, behavioral health, and long-term care services. AHCA also competitively selected dental managed care plans to provide dental services for adults and children. Recipients will enroll in one plan for their medical, behavioral, and long-term care services and a second plan for their dental services.
The new contracts contain major program improvements that will greatly benefit recipients and providers. Some of the most noteworthy benefits include:
Recipients
- Double the primary care providers in each network
- Guaranteed access to afterhours care and, where available, telemedicine
- Higher standards and accountability for transportation services
- More than 55 expanded benefits offered by health plans and extensive adult dental benefits offered by dental plans
- Smoother process for complaints, grievances, and appeals
Providers
- More pediatric physicians participating in the Medicaid Physician Incentive Program, which pays providers at the Medicare rate
- Plans will complete credentialing of providers seeking to join a plan’s network in 60 days
- Prompt authorization of services
- Smoother process for complaints, grievances, and appeals
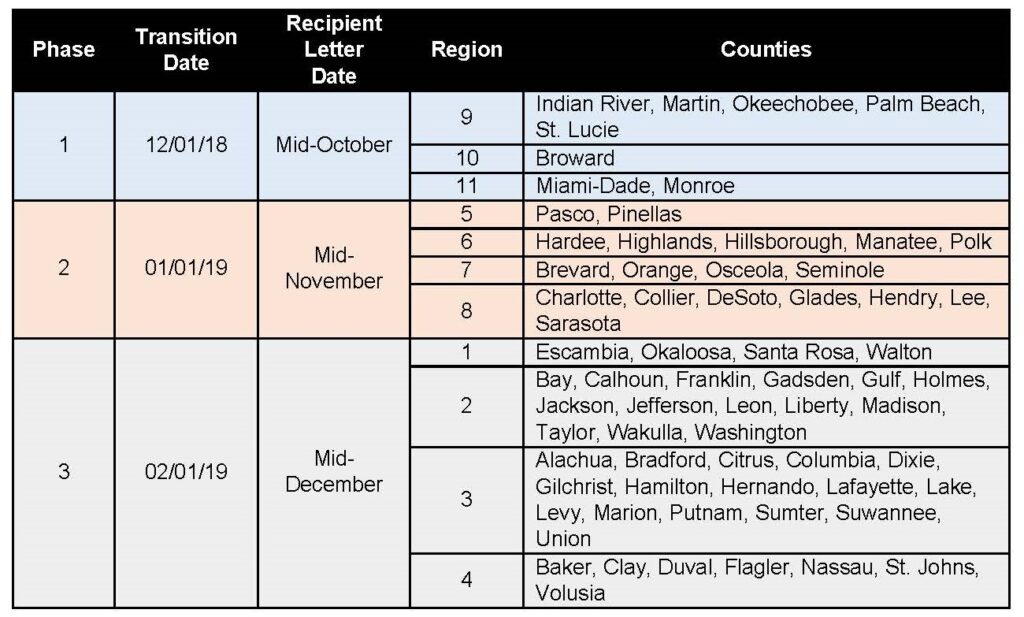
AHCA will transition to the new contracts through a regional phased rollout. During this transition, enrollees and new recipients will receive letters with specific enrollment information and needed action approximately 45 days prior to each phase going live. The chart below shows when AHCA will transition to the new contracts and when letters will be sent for each Medicaid region.
Below are links to resources about changes to the SMMC program:
- SMMC Homepage
- Medicaid Recipient Web Portal
- Choose and Enroll in a Health Plan
- SMMC Outreach and Presentation Documents
- Sign up for Program Updates
- Plan Contacts for Providers
- Plans by Medicaid Region
- Report a Complaint
- Submit Questions to AHCA